‘Like ripping my insides’ – fears hysteroscopy guidelines not enough
Wendy McLean was due to start her seventh round of IVF when her doctor said she needed a hysteroscopy – a procedure to examine the inside of her uterus.
“It was sold to me as a smear test, basically. A thin narrow camera up through your cervix.
“It’ll take minutes. You won’t need pain relief. You’ll be absolutely fine,” she said.
Wendy, 38, took over-the-counter pain killers before the outpatient procedure at Aberdeen Royal Infirmary in case it was uncomfortable, but this did not prepare her for what happened.
‘Clawed, like sharp nails’
“It felt like getting a hot poker, like getting my insides ripped out. I think I described it to somebody before as like being clawed, like sharp nails, just ripping at my insides.”
Wendy said she lost consciousness twice, vomited and asked for the procedure to be stopped.
It was only when searching online she discovered thousands of other women had had similar experiences of painful hysteroscopies without anaesthetic.
NHS Grampian said they were sorry to hear about Wendy’s experience and encouraged her to get in touch with their feedback team.
“It shouldn’t be happening,” Ms McLean said. “I never realised it was happening to so many people. I thought I was a rarity, I thought I was different and awkward and I was embarrassed.”
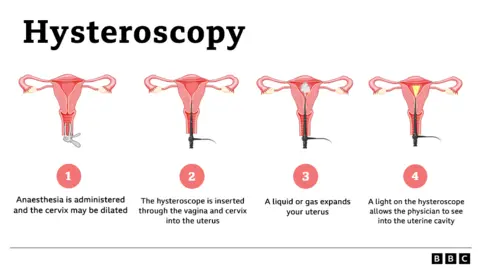
What is a hysteroscopy?
A hysteroscopy is a procedure to examine the inside of the uterus by passing a thin telescope-like device through the cervix.
It’s described as the “gold standard” in diagnosing gynaecological conditions – including cancer.
It is used to investigate problems like heavy periods and post-menopausal bleeding. Doctors can also perform biopsies and remove fibroids or polyps.
According to the Royal College of Obstetricians and Gynaecologists (RCOG), a third of those undergoing a hysteroscopy report pain levels of seven or above out of 10.
It says patients should be offered local or general anaesthesia for the procedure and their medical history should be taken into account, including trauma or difficulty with smear tests.
But despite RCOG producing new clinical guidelines promoting pain relief and choice, many women say they are not being offered it.
Procedure was stopped

May Hooper was scheduled to have an ultrasound to investigate post-menopausal bleeding at Stobhill hospital in Glasgow in July 2022.
During the procedure she was told further investigations were needed, but she said she was not told she was having a hysteroscopy or offered pain relief.
“It’s indescribable,” she said. “I really felt as though I was in a medieval torture chamber. That’s how it felt. It’s just that, I can’t believe you’re doing that to women. I had every indication under the sun for them not to do that.”
Ms Hooper asked for the procedure to be stopped and it was rescheduled – this time under general anaesthetic. The 73-year-old has complained to her health board, NHS Greater Glasgow and Clyde (NHSGGC).
She is now fighting for women to be given more information about the risk of pain and pain relief options – including general anaesthetic.
“It is a very important diagnostic procedure, absolutely, but it does not have to be painful. This is 2024 – we’re not living in the 1600s.”
NHSGGC told BBC Scotland News it would not comment on an individual case but said it followed all appropriate national guidelines while striving to ensure patients’ needs were met as treatments progress, with alternative pathways available if required.

Dr Lucky Saraswat is a consultant gynaecologist in Aberdeen, who trains doctors on how to perform hysteroscopies. She says the procedure is not painful for the vast majority of women but it’s important for patients to know they are in control.
She said: “We just have to help people make an informed choice of how they want to do it.
“Some people wouldn’t want to have an anaesthetic, as the anaesthetic is not without risks either. So, a lot of people choose to have it done in outpatient settings. Some will make a choice of having an anaesthetic.”
Campaigners claim the new clinical Green Top Guidelines minimise the risk of pain that patients may experience.
Dr Geeta Kumar, consultant gynaecologist and vice president of RCOG, said they had listened to patients’ concerns.
“Clear accurate written and verbal information must be provided, both at the time of referral, and at the procedure appointment,” she said.
“This will support a woman to make an informed choice, including whether they want to proceed with the procedure and if so, their preferences for treatment setting and pain relief options.”
Katharine Tylko, from the Campaign Against Painful Hysteroscopy, said: “It will have no impact whatsoever, apart from a few very conscientious and compassionate fighting-types of gynaecologist – young women who will say – ‘We want decent care for our patients.’
“These guidelines are not mandatory.”