Family unable to grieve after ‘hospital nightmare’
 Rachael Evans
Rachael EvansA woman says her family have been unable to grieve the death of her grandmother after a “hospital nightmare”.
Lilian Evans, 90, was taken to Wrexham Maelor hospital on 25 August after vomiting blood, but A&E staff admitted her for a UTI she did not have, said her granddaughter.
Rachael Evans, 37, said the lack of care given to her grandmother was “unbelievable” – including giving her penicillin despite an allergy and diagnosing her with cancer and Parkinson’s disease without informing the family.
Betsi Cadwaladr University Health Board apologised for the failures.
Rachael, from Wrexham, said her grandmother was an independent woman who loved her King Charles Spaniel, Meg.
Lilian, who celebrated her 90th birthday the week before she was admitted to hospital, walked three times a day – even after Meg had to be put down.
Rachael said Lilian had dementia and gave A&E staff incorrect information when she arrived – something she discovered after applying for her grandmother’s records after she died.
“There was not one test that showed that she had a UTI, they completely glossed over the fact that she was vomiting blood,” said Rachael.
“That didn’t seem to be an issue for them, and they just went along with it even though they wrote down that she didn’t have any symptoms of the UTI.”
Rachael said he gran was “fully continent” before she went to hospital.
“When we went in the next morning, she was in a huge pad – not even a nappy, it didn’t close on either side.”
Lilian lost her appetite and so she was fed nutrient-rich drinks, but cream gave her stomach-aches so they requested the juice ones.
“Whenever we’d go, they’d have the cream ones in front of her for her to drink. I kept saying these are going to make her sick and give her a stomach ache,” Rachael said.
“The nurses would make her down them.”
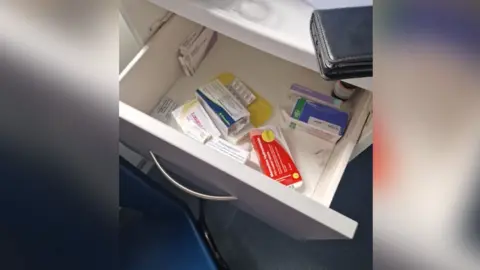
Lilian’s medication was left in an unlocked cabinet, some of which “could have seriously hurt somebody if they’d taken them”, said Rachael.
She repeatedly asked staff to lock them away, but would find them still unlocked.
Rachael said she found out her grandmother was on end-of-life care when she happened to ask a hospital staff member how she was doing, despite nobody informing the family.
“It was absolutely horrific,” she said.
“Every day we’d go and there’d be something else.
“If I didn’t have the evidence here, I don’t think anybody would actually believe us as to what actually went on there.”
 Family Photo
Family PhotoIn the days leading up to Lilian’s death, a fellow patient tested positive for Covid.
Lilian was given a lateral flow test on 18 September which was positive, then a second report said the same test had been registered in error – “please ignore”, it said.
“They went on to give her blood thinning injections, and she started vomiting up blood again,” Rachael said.
“If she didn’t have Covid, she wouldn’t have needed the blood thinning injections, she wouldn’t have started bringing up the blood again.”
On the 20 September Lilian died, the cause of death given as pneumonia.
“The issue surrounding her death was very suspicious to me. I still haven’t got to the bottom of it,” said Rachael.
When Rachael and her family received Lilian’s hospital records they discovered she had been “on an intensive cancer management plan”.
In the notes of a physiotherapist that she had been diagnosed with Parkinson’s disease and had received blood tests which indicated she had a heart attack, which Rachael said they had no idea about.
“We still don’t know if she did or if she didn’t, because the hospital are now refusing to answer my questions,” she said.
As well as this, the records show on the night Lilian died at about 22:00, the night staff signed to say they had checked on her at 00:30, 03:30 and 06:30 the next morning.
This leads Rachael to believe staff signed the form at the start of their shift so they did not have to check on Lilian again.
“This was heart-breaking as my gran was very anxious so to think of her on her own shouting for help and not getting any is awful,” Rachael said.
 Rachael Evans
Rachael EvansThe records also showed that despite A&E staff noting Lilian was able to make her own decisions, a nurse later applied for a Deprivation of Liberty Safeguards order.
An assessment was taken and it was decided Lilian did not need this, however in following reports staff mention one being in place.
Rachael, her mother, father and uncle all have power of attorney, but they were not told, Rachael said.
In July she had a meeting with the health board after complaining about her grandmother’s care.
She said they tried to “gloss over” the problems and told her they would “look into it” but after 11 weeks told her they were not going to answer her questions.
Rachael said the hospital’s communication and documentation were “really bad” – often getting Lilian’s name and details wrong.
“This has taken over – just waiting – it’s been over a year now since my gran died, and we’ve still not got all of the answers.
“It is very difficult to grieve when you don’t really know what’s happened – they didn’t tell us anything when she was in hospital, and now they’re refusing to tell us after she’s died.”
Carol Shillabeer, chief executive of Betsi, said: “On behalf of the Health Board I sincerely apologise to Ms Evans’ family for the failures identified in her care and treatment, we fell short of the standard that should be expected.”
The case has been referred to the ombudsman, who has been approached for comment.








