Women ‘traumatised’ after lack of infertility support
 BBC
BBCA woman says she was left “traumatised” by the lack of care she received after a miscarriage.
Shelley Romaniuk, 33, was told she had miscarried while attending a 12-week scan, and says she was left alone with no support from health services.
Research shows infertility-related trauma is more common than previously thought, with women not being offered enough mental health support.
The Welsh government said fertility clinics used by the NHS in Wales must offer an opportunity to talk to a counsellor before treatment starts, and anyone who needs further help should request a referral via their GP.
Article contains details some readers may find distressing
Shelley and her husband found out they were expecting their first child nine years ago, and attended their routine scan without realising they had already lost the baby – a missed miscarriage.
“We went for the 12-week scan, and we were informed the baby had no heartbeat.
“After that scan we were just put into a room, given a leaflet and just left there until someone came into ask what we wanted to do”, she added.
Shelley says she wanted a surgical procedure called dilation and curettage (D&C) to remove the baby, but was told that could not happen for a week because there were no available appointments.
“They basically said you can’t have it now, you have to go home and come back in a week and that was it,” she said.
“There was no offer of support, no therapy, no counselling, and you’re walking away carrying your baby who’s no longer alive.”
‘We were asking for help continuously’
While waiting for the D&C procedure, Shelley started experiencing cramps at home and went to A&E.
“I didn’t make it to the D&C, unfortunately I lost the baby naturally.
“But even after that, we went through the whole process, I was sent on my merry way and there was zero support.
“I was depressed for a long time after that.”
After years of trying to conceive naturally, Shelley and her husband decided to seek private fertility treatment, and the couple are now expecting a baby girl in a few weeks.
But Shelley believes the lack of mental health support she received made conceiving harder.
“We were asking for help continuously, but there was nothing,” she said.
“The trauma left from that missed miscarriage and how we were treated stays with you.
“Even now going for scans it’s rough, it brings it all back.
“Maybe if I had support to deal with that and move forward and process that trauma, maybe things would have been different.”
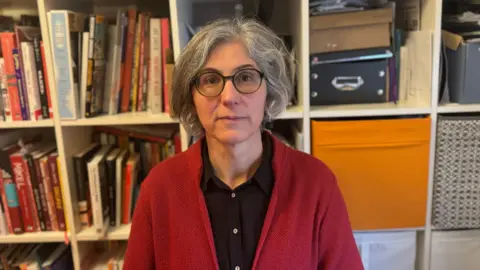
 Shelley Romaniuk
Shelley RomaniukResearch by Fertility Network UK, Cardiff University, Cardiff Metropolitan University and Queen’s University Belfast found 41% of respondents from across the UK were diagnosed with post-traumatic stress disorder (PTSD) after experiencing infertility.
Dr Catherine Hill from the charity said: “This research is very important, because it confirms what people working in the fertility sector have suspected for a while, and that is that infertility-related trauma is very common, and it’s a silent trauma within our society.”
In Wales specifically, Dr Hill said many respondents said they had only been offered one session of counselling during their fertility journey.
“One session of counselling tends to not even scratch the surface, and many clinics offer more than that.”
The research also found that long waits for fertility tests and investigations in Wales were adding to people’s trauma.
Lead researcher Dr Sofia Gameiro from Cardiff University said the care many participants received while accessing fertility treatment exacerbated their trauma, and in some cases caused their trauma.
“While some respondents reported positive, skilful and compassionate care, it was clear that over 60% highlighted aspects of the care they received caused or amplified trauma,” she said.
This included a lack of empathy or acknowledgment of distressing experiences, conflicting advice and unsupportive care when receiving bad news.
A Welsh government spokesperson said they recognised that infertility and waiting for treatment can have a significant impact on people’s mental health and wellbeing.
“Two rounds of NHS IVF treatment are available to qualified patients, as per criteria set by the NHS Wales Joint Commissioning Committee,” they said.
“The committee ensures that specialised services provide robust, high-quality care which is safe for patients and cost effective for the NHS.”







