Gynaecology waiting lists double, leaving women in pain
 BBC
BBCWaiting lists for gynaecology appointments across the UK have more than doubled since February 2020, BBC research reveals.
Records show around three-quarters of a million (755,046) women’s health appointments are waiting to happen – up from 360,400 just before the pandemic.
This would suggest around 630,000 people – at the very least – are on the list to be seen for problems that range from fibroids and endometriosis to incontinence and menopause care.
Health ministers across the UK say they are working on plans to improve the situation, but health leaders say that women are being let down.
‘The illness controls my whole life’
 Anna Cooper
Anna CooperAnna Cooper, 31, from near Wrexham in North Wales, has had severe endometriosis since her teens.
The condition – where tissue similar to the lining of the womb grows outside it – has left her with permanent organ damage.
She has had to have 17 operations, including a hysterectomy to remove her womb.
She also has two stomas in place for life because much of her bladder and bowel have had to be removed. She lives with her partner and young daughter.
“The disease controls my social life, my work life and my ability to function every day.
“It is not just a period problem – it is a whole body problem. It ripples through your body,” she says.
 Anna Cooper
Anna CooperThe BBC spoke to her in 2023 about setting up her own charity, Menstrual Health Project.
A year on, she says she is still in pain and is on the NHS waiting list yet again because she has experienced bleeding after her hysterectomy.
Anna wears a morphine patch to help deal with pain every day.
But for years, she says medics did not listen to her, and told her the pain was “in her head” and that she had to “just get used to it”.
She feels getting a diagnosis sooner would have changed her life: “The delay in my care has cost me some of my major organs.
“Doctors have told me that if they’d caught it sooner, I wouldn’t have ended up the way I am, living with two stomas and being in early menopause at the age of 31.”
In the last three years she made the decision to spend £25,000 on private operations, borrowing money to help.
She counts herself lucky to get private care but feels she was “almost left with no choice” because the waiting lists are so long: “I can be a mum who isn’t just in her bed constantly because she is crippled with pain.”
Endometriosis has “mentally tormented” her for the most of her adult life.
“It is really difficult dealing with a condition where I look absolutely fine from the outside, but internally, I’m just in despair.”
‘Lack of priority’
“Women are being let down” and change is “urgently needed,” says Dr Ranee Thakar, president of the Royal College of Obstetricians and Gynaecologists (RCOG).
The college’s new report looks at the impact on people waiting for care.
“Gynaecology is the only elective speciality that solely treats women and has one of the worst waiting lists across the UK.
“This reflects the persistent lack of priority given to women and women’s health, ” Dr Thakar says.
“Women are suffering. We know it is affecting their mental health. They are not able to go to work, they are not able to socialize.”
Dr Thakar adds that if the women had been treated earlier, their conditions wouldn’t have progressed as much, and they would continue to contribute to society.
A recent report led by the NHS Confederation suggests being absent from work because of heavy periods, endometriosis, fibroids and ovarian cysts costs the UK economy nearly £11 billion each year.
The RCOG is calling for governments to commit more long-term funding, to ensure people get the help they need.
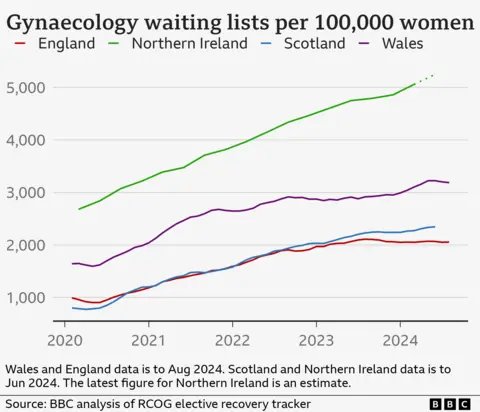
There are some signs that waiting lists are starting to improve.
Waits have not been rising as steeply this year and NHS England’s latest figures show there has been a drop in numbers on the waiting list of over 4,700 compared to the month before.
But the situation is still much worse than pre-pandemic. In Feb 2020 there were 66 gynaecology waits of more than a year. Now there are more than 22,000.
Dr Sue Mann, NHS England’s national clinical director for women’s health, acknowledged some women wait too long for crucial gynaecology appointments, despite staff working hard to see more patients.
She says one way of helping is specialist teams working outside of hospitals.
“Some of these conditions can be managed very well by specialist healthcare teams in the community, which is why we are expanding neighbourhood women’s health hubs in every local care system across the country.”
In Wales, the government plans to publish a women’s health plan next month.
“A 10-year Women’s Health Plan is being developed to drive the improvement needed to provide good quality health services to women throughout their lifetime,” a Welsh Government spokesperson said.
Regions in Northern Ireland are working on plans to improve gynaecology services, taking on the 20 recommendations made in a recent report.
The department of health says some will require “additional funding and lead-in time.”
Scotland’s Women’s Health Minister Jenni Minto said excessively long waits were not acceptable and more money was going towards women’s health.
“That is why one of the initial priorities of the women’s health plan is to improve access for women to appropriate support, diagnosis and treatment.”
 Anna Cooper
Anna CooperAnna Cooper is hoping ministers “follow through with their words”.
When governments say they are going to prioritize women’s health, then they need to show they are doing just that, she says.
“Currently they are not showing it, and this is people’s lives we are rolling the dice on… And having a daughter, I really fear for young girls’ and women’s futures.”
How we arrived at the figures
To estimate the size of the gynaecology waiting list for the UK we added together the most recent figures available for all four nations, as tracked by the RCOG.
This includes waits for gynaecology appointments and planned procedures and excludes urgent appointments for things like suspected cancer.
It tells you how big the waiting list is, but some patients may need more than one appointment.
Our estimate for the number of people waiting is at least 634,239 – and it could be considerably more.
We worked this out by looking at data from the NHS in England that suggests across waiting lists there is around a 16% difference between the number of appointments and people waiting.
We have applied this to the gynaecology waiting list.
It could underestimate the size of the problem, as gynaecology patients are less likely to be waiting for two appointments than patients in some other specialities.
Additional reporting by Vicki Loader, Catherine Snowdon and Alison Benjamin







